Asthma is one of the most common chronic illnesses in children. In everyday clinical practice, we see many different presentations, which can sometimes make diagnosis and management confusing. A practical, bedside-based discussion using real-life scenarios often helps us understand asthma better and improves patient care.
Some Common Clinical Scenarios
Let us start with three real-life situations that clinicians frequently encounter:
A 4-year-old child with recurrent episodes of cough and wheeze occurring once every two months, usually with fever and cold, and completely well in between episodes.
A 9-year-old child referred for spirometry to “confirm” a diagnosis of asthma.
A 13-year-old child with very high fractional exhaled nitric oxide (FeNO) levels (195), referred for review of diagnosis and further management.
These scenarios highlight how varied asthma presentations can be and why careful assessment is essential.
Gravity of the problem
Around 14% of children worldwide suffer from asthma.
It causes significant morbidity, affects school attendance, family life, and overall quality of life.
Despite available treatments, asthma management remains suboptimal, even in developed countries.
Optimised care is crucial so that children with asthma can lead normal, active lives.
Childhood Asthma- A Bedside Approach
Definition
Asthma is the most common chronic inflammatory disease of the lungs in children. It is a heterogeneous condition, meaning it can vary greatly between individuals.
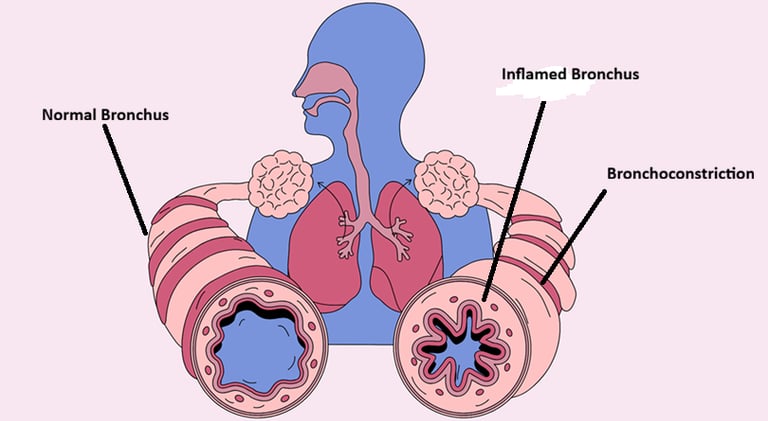
Three key processes occur in asthma:
Reversible bronchoconstriction (narrowing of airways)
Chronic airway inflammation
Increased mucus (secretions)
Basic Pathophysiology
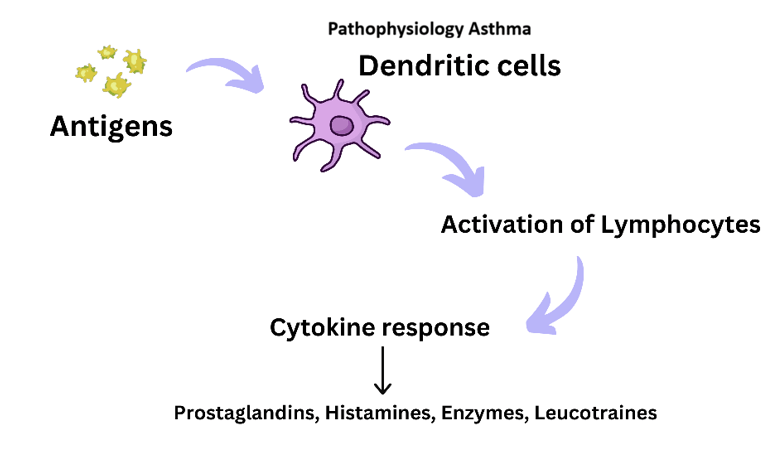
When a trigger is present:
The immune system is activated.
Dendritic cells stimulate T-lymphocytes.
Inflammatory mediators such as histamine, leukotrienes, prostaglandins, and enzymes are released.
This leads to:
Airway narrowing
Swelling of airway lining
Increased mucus production
The final result is airflow obstruction, which causes asthma symptoms.
Very basic at Cellular Levels


Trigger Factors and Risk Factors
Identifying trigger factors is a key part of history-taking. Common triggers include:
Viral infections
Allergens (dust mites, pollen, pets)
Exercise
Cold air
Smoke and pollution
Risk factors help guide long-term management and prevention strategies. Identifying and avoiding triggers, where possible, can significantly improve asthma control.
Clinical Presentation
Typical symptoms include:
Recurrent cough (often dry)
Wheezing
Shortness of breath
Chest tightness
A supportive family history of asthma or atopy strengthens the clinical suspicion.
Diagnosis !
1. History – The Most Important Tool
The diagnosis of asthma is primarily clinical. Investigations support the diagnosis but do not replace a good history.
2. Spirometry
Spirometry measures lung function, especially how much air a child can blow out.
FEV₁: Air exhaled in the first second
FVC: Total air exhaled
FEV₁/FVC ratio:
75% is usually normal
<75% suggests airway obstruction
If obstruction is present, a reversibility test is performed after giving a bronchodilator. An improvement of ≥12% supports asthma diagnosis.
Important points:
Normal spirometry does not exclude asthma
The child may be asymptomatic during testing
Asthma is not the only cause of airway obstruction
3. Fractional Exhaled Nitric Oxide (FeNO)
FeNO measures nitric oxide released during allergic airway inflammation.
Can be performed in children as young as 3 years
Helps assess airway inflammation
Has moderate diagnostic accuracy
Useful in monitoring treatment response
However:
FeNO can be falsely elevated in certain conditions
High FeNO alone does not confirm asthma
Test technique and clinical context are crucial.
4. Allergy Testing
Allergy testing helps identify trigger factors, not diagnose asthma.
Blood eosinophils may support allergic inflammation
Specific allergy testing is useful when triggers are suspected
Results can guide avoidance and management strategies.
Revisiting the Three Clinical Scenarios
4-year-old with episodic wheeze
Most likely recurrent viral-induced wheeze. No clear evidence of asthma at present.9-year-old referred for spirometry
Spirometry is helpful, but diagnosis depends mainly on history. Normal spirometry does not rule out asthma.13-year-old with very high FeNO
Despite high FeNO, the child had no symptoms and was on regular preventer treatment. This raises questions about:Test accuracy
Technique
Whether FeNO alone should guide diagnosis
Principles of Asthma Management
Asthma management is not just about medication—it includes:
Detailed history
Appropriate investigations
Individualised treatment plan
Regular follow-up
Key principles:
Avoid trigger factors where possible
Treat airway inflammation
Inhaled corticosteroids for long-term control
Systemic steroids for acute attacks
Treat bronchoconstriction
Bronchodilators for symptom relief
Leukotriene modifiers (e.g., montelukast) can help selected patients
There is one thing above all -
Education, Education and Education for all of us and parents.
